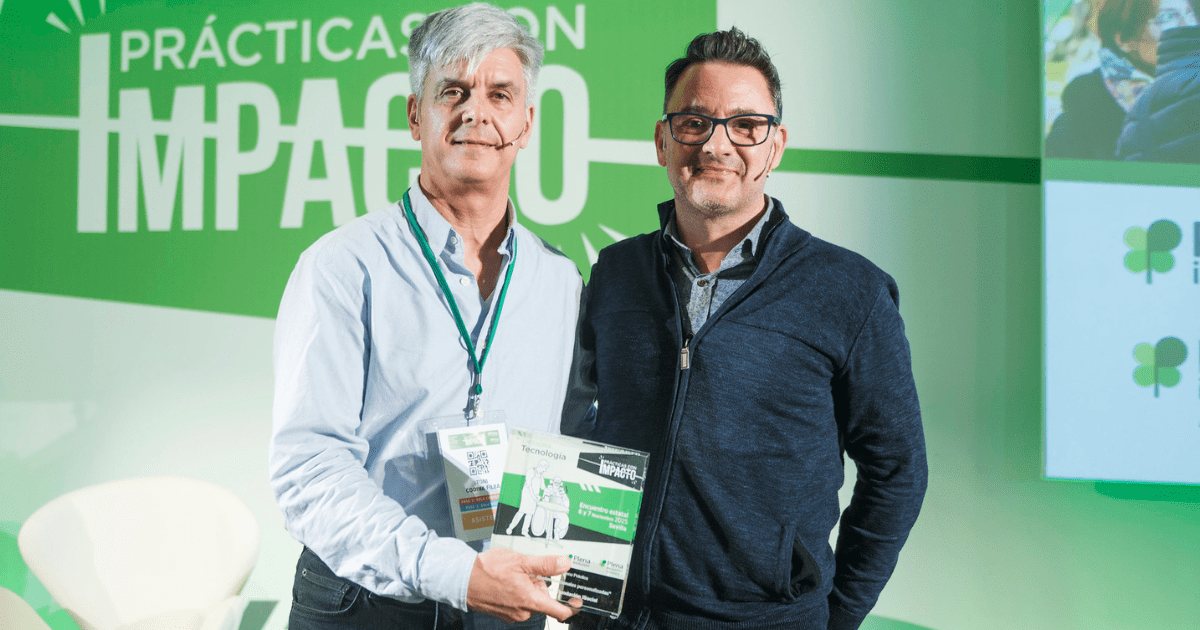
Jordi Amat is the Director of the Information and Communication Technologies Area at the Department of Social Rights and Inclusion of the Government of Catalonia. In this role, he drives the transformation of social services through projects like wSocial, an innovative tool that supports social intervention carried out by Basic Social Services Areas, facilitates case diagnosis and management, and promotes a comprehensive view of the citizen’s situation. We speak with him to learn more about wSocial, how it works, and its planned rollout.
What is wSocial and what need does it address?
wSocial is a tool that supports social intervention carried out by the Basic Social Services Areas, which are the local units —sometimes consortia— of municipalities that manage social services. To understand what wSocial is, one must first understand how these areas operate.
We can draw a parallel, cautiously, with the healthcare system: just as someone with a health issue goes to a primary care center (CAP), someone with a social issue can go to a Basic Social Services Area. The citizen requests an appointment, and the team, following protocols and relying on their experience, diagnoses the situation: it could be a case of violence, lack of housing, need for financial assistance, etc. Once the diagnosis is made, a work plan is defined to help the person improve their situation and access a dignified life. This plan may include services or benefits provided by the municipality, the regional government, or the state.
How does wSocial support this process?
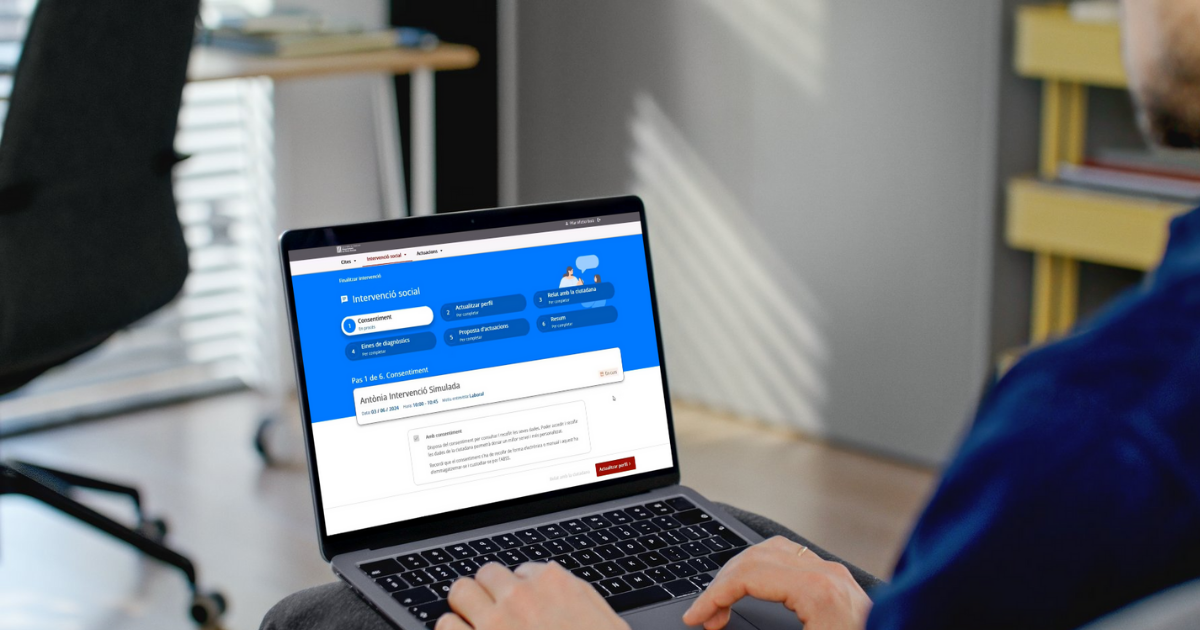
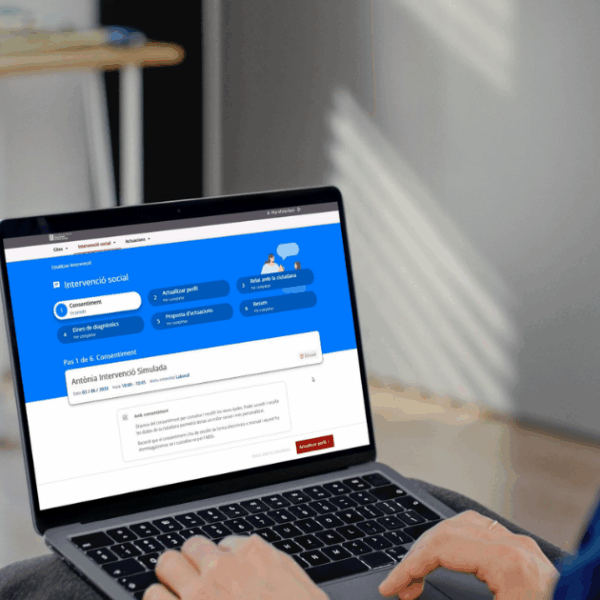
wSocial aims to support this task by placing the citizen and their household at the center of the intervention. To achieve this, the Department of Social Rights has collaborated with the social ecosystem (including social entities, TIC Salut, and the Basic Areas themselves) to define a dictionary of social needs based on the SNOMED standard, which is already used in the healthcare field. The goal of this standard is to standardize language and diagnostic protocols.
Additionally, wSocial provides a 360º view of the person’s situation by gathering information from different Basic Areas —for example, if the person moves to another municipality. It offers a viewer of all the information that basic social services have about a person, which is often scattered across municipalities. This prevents the citizen from having to repeat their story or submit the same documents to each new service, and allows social workers to make better diagnoses.
So, is it about unifying dispersed social information?
Exactly. Today, there are already tools that offer some level of interoperability, but wSocial proposes to unify everything into a single platform shared by all Basic Areas. It would be like a social version of “La Meva Salut,” accessible —with the person’s consent— to social services professionals. The system includes mechanisms to manage this consent rigorously.
A major milestone has been the exchange of viewers between the health and social sectors. This allows social professionals to access basic health information without requesting reports, and health professionals to consult social data. This way, information is shared more efficiently without duplicating efforts.
How is the third sector integrated into wSocial?
wSocial is a tool for social professionals, with data coming from this 360º view of the citizen, collected in the eSocial platform, which stores all the information. Naturally, the third social sector is another actor in the social ecosystem, either as a provider or as a parallel and complementary actor. Therefore, sharing information with them is essential, while also respecting legal frameworks and the General Data Protection Regulation (GDPR).
wSocial is a tool for social professionals, with data coming from this 360º view of the citizen, collected in the eSocial platform, which stores all the information. Naturally, the third social sector is another actor in the social ecosystem, either as a provider or as a parallel and complementary actor. Therefore, sharing information with them is essential, while also respecting legal frameworks and the General Data Protection Regulation (GDPR).
wSocial incorporates artificial intelligence. How does it work?
We’ve implemented two AI tools. The first is already in production: it’s a generative AI that detects potential needs based on the conversation between the citizen and the social worker. The professional writes the narrative, and the AI suggests identified situations and possible additional ones. It’s a support tool, but the final judgment always lies with the professional.
This tool has proven to be scalable and efficient: it can support the equivalent of 1.5 million interviews, with an estimated load of 6,000 interviews per morning.
The second tool, still in pilot phase, is for automatic transcription and translation. It allows the professional and the citizen to maintain eye contact, as it translates and transcribes in real time in languages such as Catalan, Spanish, English, and Egyptian Arabic. The current result has very low latency (2 seconds), making it useful and scalable.
Are other automated features planned?
Yes. Through the information hub —called dSocial— we’ve created a “sentinel” system that detects situations where a citizen could be receiving a benefit but isn’t. Always with the citizen’s authorization, of course.
There’s also a project using anonymized data that cross-references health and social information to predict future needs. This helps better understand the evolving profile of citizens served in the social domain.
What stage is wSocial currently at?
We already have a first version of the tool. The Department’s goal is to continue evolving it and adding improvements across different areas.
This first version has focused heavily on facilitating diagnosis, highlighting the work done to standardize and harmonize the identification of vulnerability situations, especially through SNOMED. The use of AI to consistently identify situations and support social workers is already underway, as are the transcription and translation tools. At this stage, we’ve paid close attention to improving citizen care. There’s still testing to be done.
What are the future prospects?
A next step is to integrate all telecare systems from the Basic Areas.
Our roadmap for this year is very ambitious: we want to incorporate all this information. Our goal is for this data to serve the entire community —the entire social ecosystem we mentioned earlier. We also aim to integrate the 109 Basic Areas, which currently have their own systems, so they can manage assistance directly. We want to incorporate all existing diagnostic tools and any new ones that may emerge.
wSocial also aims to facilitate the standardization of all Basic Areas, supporting tasks such as writing social reports or meeting other needs. It will provide standardized formats and help fill in data, since this data will already be in the system. And, given that all Basic Areas have a program contract with the Department of Social Rights, another goal is to make these contracts easier to complete in the future, as much of the required information will already be in the system.
When is the full rollout of wSocial expected?
During 2025. A support plan has already been developed with territorial services and some Basic Areas to ease the migration from current systems. Everything is ready, and the rollout is underway.